It was a typical Tuesday morning when the dull ache in my lower back intensified, sending a shooting pain down my leg. I had been experiencing this discomfort for a few weeks, but it suddenly felt unbearable. After a visit to my doctor, I received a diagnosis that sent a shiver down my spine: a minimal posterior disc bulge. While the term itself was unfamiliar, I was quickly learning that my back pain was not a mere inconvenience but a potential sign of a significant issue.
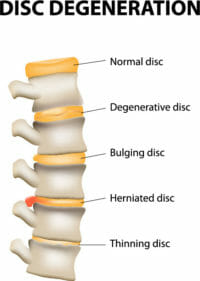
Image: yodack.com
As my doctor explained, a disc bulge is a common condition that occurs when the soft, jelly-like center of an intervertebral disc, known as the nucleus pulposus, pushes beyond the outer fibrous ring, called the annulus fibrosus. While this might sound alarming, a minimal posterior disc bulge often does not cause any noticeable symptoms and resolves on its own. However, the experience left me wanting to understand more about this condition, and I set out to learn everything I could about minimal posterior disc bulges.
Understanding Minimal Posterior Disc Bulges
A minimal posterior disc bulge refers to a small protrusion of the intervertebral disc tissue, specifically in the back of the spine. This bulge can affect any part of the spine, including the cervical (neck), thoracic (mid-back), and lumbar (lower back) regions. It is important to note that a minimal posterior disc bulge is not necessarily a painful condition. In fact, many individuals with this condition may experience no symptoms at all.
One of the main reasons why a minimal posterior disc bulge may go unnoticed is its size. Unlike a herniated disc, where the nucleus pulposus ruptures through the annulus fibrosus, a minimal posterior disc bulge involves a small, localized protrusion. This protrusion may not be severe enough to compress nearby nerves or cause pain. However, as the condition progresses, the disc bulge can become larger, potentially leading to symptoms such as back pain, leg pain, numbness, or weakness.
Factors Contributing to Minimal Posterior Disc Bulges
While the exact cause of a minimal posterior disc bulge is not always clear, several factors can contribute to its development. Some of the most common contributors include:
- Age: As we age, the intervertebral discs naturally lose water content, making them more susceptible to degeneration and bulging.
- Repetitive movements: Engaging in activities that involve repetitive stress on the spine, such as lifting heavy objects, can contribute to disc bulges.
- Trauma: A sudden injury, such as a fall or car accident, can also damage the intervertebral discs and lead to a bulging disc.
- Genetics: Some individuals may have a genetic predisposition for disc degeneration and bulging.
- Poor posture: Maintaining poor posture for extended periods can strain the spine and increase the risk of a disc bulge.
- Obesity: Excess weight puts extra stress on the spine, making discs more vulnerable to bulging.
Symptoms of Minimal Posterior Disc Bulges
As mentioned earlier, minimal posterior disc bulges often cause no symptoms. However, if the bulge becomes larger or presses on nearby nerves, it can lead to a range of symptoms, including:
- Back Pain: A common symptom of a minimal posterior disc bulge is localized back pain. The pain may be dull, aching, or sharp, and it might radiate to other areas, such as the buttocks or legs.
- Leg Pain: If the bulge press on nerves in the spine, it can cause pain that radiates into the legs, commonly referred to as sciatica. This pain may be shooting, burning, or tingling.
- Numbness or Weakness: A minimal posterior disc bulge can also cause numbness or weakness in the legs or feet, depending on the location and severity of the bulge.
- Tightness or Stiffness: The muscles around the affected area may feel tight or stiff, making it difficult to bend or move.

Image: polizintra.weebly.com
Diagnosis and Treatment
To diagnose a minimal posterior disc bulge, a doctor will typically begin by reviewing the patient’s medical history and conducting a physical examination. This may involve assessing the patient’s range of motion, muscle strength, and reflexes.
Imaging tests such as an X-ray or MRI scan are often used to confirm the diagnosis and assess the severity of the disc bulge. X-rays can reveal any changes in the alignment of the spine or the presence of bone spurs. An MRI scan can provide a more detailed image of the soft tissues, including the intervertebral discs, and can help distinguish between a disc bulge, a herniated disc, and other potential causes of back pain.
Management Options
The treatment for a minimal posterior disc bulge will depend on the severity of the symptoms, the location of the bulge, and the individual patient’s overall health. In many cases, conservative treatments are effective in managing the condition and relieving symptoms. These treatments may include:
- Rest: Limiting activities that aggravate the pain is essential. This may involve avoiding heavy lifting, prolonged sitting or standing, and strenuous exercise.
- Ice and Heat Therapy: Applying ice packs to the affected area for 15-20 minutes at a time several times a day can help reduce inflammation and pain. Heat therapy can also be helpful in relaxing muscles and easing pain.
- Over-the-Counter Pain Medication: Nonsteroidal anti-inflammatory drugs (NSAIDs) such as ibuprofen or naproxen can help reduce pain and inflammation.
- Physical Therapy: A physical therapist can teach exercises to strengthen the back muscles, improve posture, and increase flexibility. They can also provide guidance on proper lifting techniques and activities that are safe for the spine.
- Injections: Corticosteroid injections can be used to reduce inflammation and pain. However, this is often a temporary solution, and the injections may not be effective in all cases.
In some cases, surgery may be recommended. This is usually reserved for patients who experience severe pain or neurological problems that do not respond to conservative treatment. Surgical procedures for a minimal posterior disc bulge typically involve removing the part of the disc that is pressing on the nerve to relieve pressure.
Expert Tips and Advice
Based on my personal experience and research, I have compiled some helpful tips and advice for those dealing with a minimal posterior disc bulge. These tips can help prevent future pain and promote healing:
- Maintain a Healthy Weight: Excess weight puts extra stress on the spine, increasing the risk of disc degeneration and bulging. Losing even a small amount of weight can have a significant impact on back pain.
- Improve Posture: Practicing proper posture is crucial for maintaining a healthy spine. Avoid slouching and make sure you have proper support for your back when sitting or standing for long periods.
- Stretch Regularly: Stretching can help improve flexibility and reduce muscle tension in the back. It is important to stretch gently and avoid any movements that cause pain.
- Engage in Low-Impact Exercise: Low-impact exercises such as swimming, walking, or cycling can help strengthen muscles, improve flexibility, and maintain a healthy weight without putting excessive stress on the spine.
- Seek Professional Guidance: If you experience back pain or other symptoms that you suspect may be related to a disc bulge, it’s essential to see a doctor. Self-treating can be dangerous, and professional guidance can help ensure proper diagnosis and treatment.
Remember that while a minimal posterior disc bulge may seem concerning, it is a relatively common condition. With proper management and care, you can effectively manage your symptoms and prevent further complications.
Frequently Asked Questions (FAQs)
Q: Is a minimal posterior disc bulge a serious condition?
A: While it can be alarming to receive this diagnosis, a minimal posterior disc bulge is not necessarily serious and often resolves on its own. However, it is important to seek medical attention if you experience any symptoms.
Q: Can a minimal posterior disc bulge be prevented?
A: While some factors like genetics are outside our control, lifestyle changes can reduce the risk of developing a disc bulge. Maintaining a healthy weight, practicing proper posture, and engaging in regular physical activity can all help.
Q: How long does it take for a minimal posterior disc bulge to heal?
A: The healing time for a minimal posterior disc bulge varies depending on the individual and the severity of the condition. With proper treatment, many people start to feel better within a few weeks, while others may take several months to fully recover.
Q: Can a minimal posterior disc bulge cause permanent damage?
A: In most cases, a minimal posterior disc bulge does not cause permanent damage. However, if it progresses to a herniated disc or causes significant nerve compression, it can lead to long-term problems. Early diagnosis and treatment can help prevent this from happening.
Minimal Posterior Disc Bulge
Conclusion
A minimal posterior disc bulge is a common condition that is often asymptomatic. Understanding the factors contributing to its development and recognizing the potential symptoms can help individuals take proactive steps to prevent or manage this condition. Maintaining a healthy lifestyle, practicing good posture, and engaging in regular exercise are essential for supporting a healthy spine and minimizing the risk of disc degeneration. Remember, if you experience any back pain or other symptoms, it’s crucial to speak with a doctor for proper evaluation and treatment.
Are you interested in learning more about managing back pain and understanding other spine health issues? Let me know in the comments below!

:max_bytes(150000):strip_icc()/OrangeGloEverydayHardwoodFloorCleaner22oz-5a95a4dd04d1cf0037cbd59c.jpeg?w=740&resize=740,414&ssl=1)




