Imagine waking up one morning with a stiff neck and a dull ache in your lower back. You stretch and try to move, but the pain persists. This isn’t a rare scenario. Many people experience this discomfort, and the culprit might be a posterior annular bulge. This seemingly harmless-sounding condition can cause significant pain and impact your daily life.
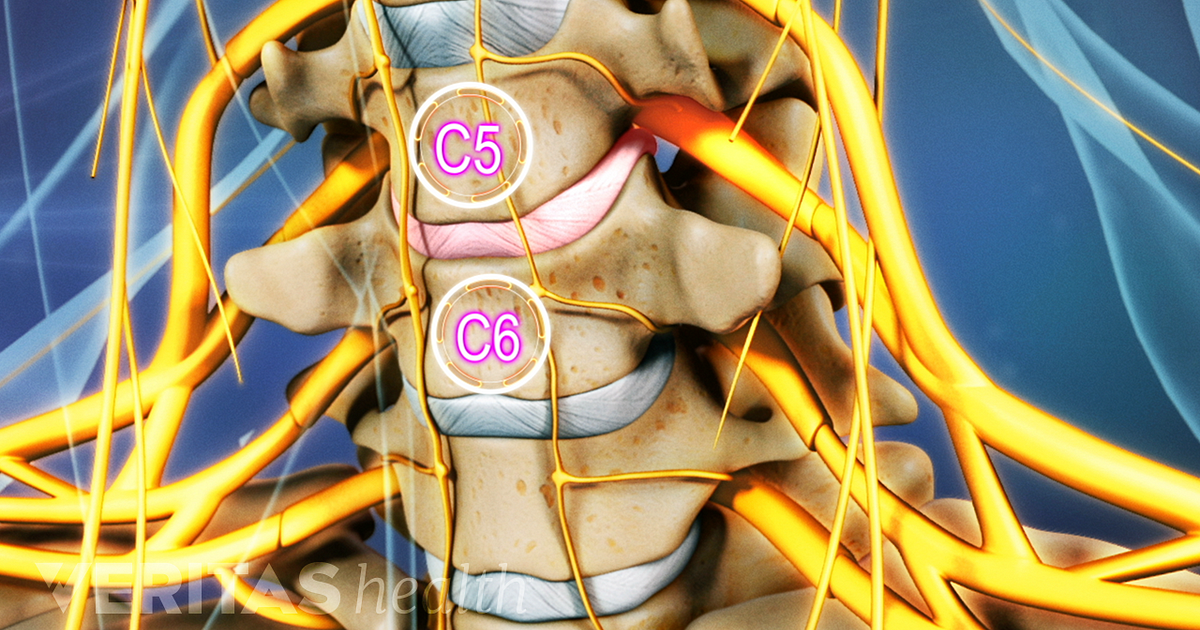
Image: www.spine-health.com
It’s normal to feel a little apprehensive when you hear a doctor mention a “bulge.” But understanding what it is and how it affects you can help ease any anxieties and guide your path toward recovery. This article will provide a comprehensive exploration of the posterior annular bulge, its causes, symptoms, and treatment options, empowering you to make informed decisions about your health.
What is a Posterior Annular Bulge?
The posterior annular bulge is a condition that affects the intervertebral discs, the cushions between the vertebrae in your spine. These discs are made of a tough outer ring called the annulus fibrosus and a soft, gelatinous inner core called the nucleus pulposus. A posterior annular bulge occurs when the annulus fibrosus weakens, allowing the nucleus pulposus to protrude backward, towards the spinal canal. This bulge can press on the spinal nerves, causing pain, numbness, and weakness.
It’s important to note that a posterior annular bulge is not the same as a herniated disc. In a herniated disc, the nucleus pulposus actually breaks through the annulus fibrosus. While a posterior annular bulge is considered less severe, it can still cause significant discomfort and requires attention.
Causes of a Posterior Annular Bulge
Several factors can contribute to the development of a posterior annular bulge, including:
Age-Related Degeneration
As we age, our intervertebral discs naturally lose water content and become less flexible. The annulus fibrosus weakens over time, making it more susceptible to bulges. This degeneration is a common factor in the development of posterior annular bulges in older individuals.
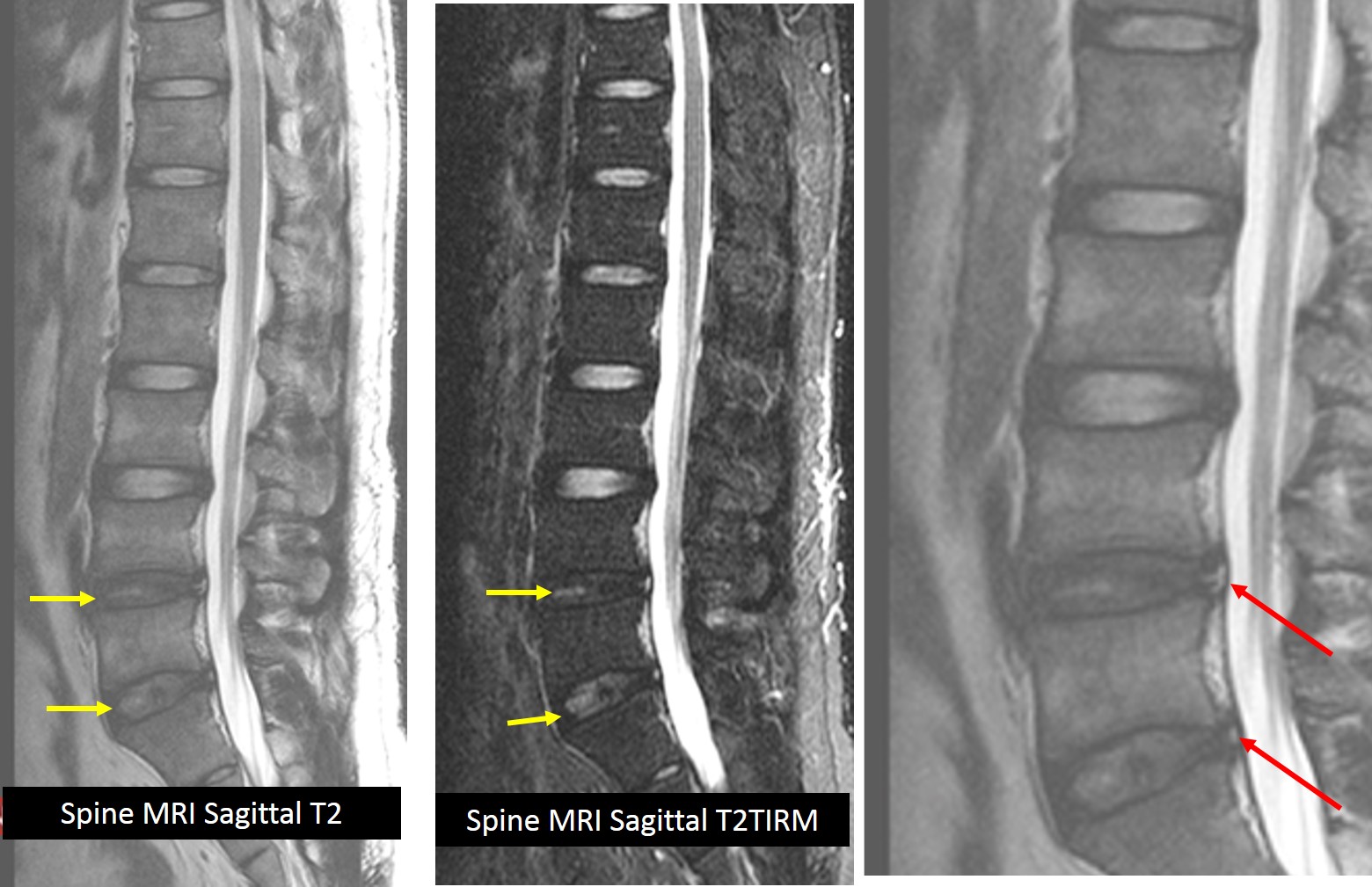
Image: radiologycases.my
Repetitive Strain
Jobs or activities that involve repetitive bending, twisting, or lifting can put stress on the intervertebral discs. This repeated strain can cause the annulus fibrosus to weaken and bulge over time. This is a common factor for people working in construction, manufacturing, or other physically demanding professions.
Trauma or Injury
A sudden impact or injury to the spine, such as a car accident or a fall, can also cause a posterior annular bulge. The impact can damage the annulus fibrosus and force the nucleus pulposus to bulge outward. This is a common cause of posterior annular bulges in younger individuals who have experienced a sudden traumatic event.
Poor Posture
Maintaining poor posture for extended periods puts constant strain on the spine, leading to disc degeneration and potential bulges. This is why it’s important to be mindful of your posture while sitting, standing, and sleeping.
Symptoms of a Posterior Annular Bulge
The symptoms of a posterior annular bulge can vary widely depending on the severity and location of the bulge. Some common symptoms include:
- Back pain: This is the most common symptom, usually localized to the area of the bulge. The pain might be sharp, dull, aching, or throbbing.
- Neck pain: Similar to back pain, pain in the neck can be a symptom of a posterior annular bulge in the cervical spine.
- Pain radiating down the legs or arms: This is known as sciatica or radiculopathy and occurs when the bulge presses on a nerve root. The pain can travel down one leg or arm, causing numbness, tingling, and weakness.
- Muscle spasms: The back muscles might spasm in an attempt to protect the affected area.
- Stiffness: The spine might feel stiff and inflexible, especially when getting up in the morning, or after prolonged sitting or standing.
- Numbness or tingling: This can occur in the area of the bulge or in the extremities, depending on the location of the affected nerve.
- Weakness: A posterior annular bulge can cause weakness in the muscles controlled by the compressed nerve.
Diagnosis of a Posterior Annular Bulge
Diagnosing a posterior annular bulge typically involves a combination of medical history, physical examination, and imaging tests. A doctor will ask about your symptoms, perform a physical examination to check your range of motion, reflexes, and muscle strength. They will also examine the spine for tenderness, muscle spasms, and other signs of nerve compression.
Imaging tests are often necessary to confirm the diagnosis and identify the location and severity of the bulge. Common imaging tests used include:
- X-ray: This can show any bone abnormalities or misalignment, but it may not clearly visualize the intervertebral discs or a bulging disc specifically.
- MRI (magnetic resonance imaging): This is the gold standard for diagnosing posterior annular bulges. MRI provides detailed images of the soft tissues, including the intervertebral discs, and can show the extent of the bulge and any nerve compression.
- CT scan (computed tomography): A CT scan can provide detailed images of the bones and soft tissues. It may be used as an alternative to MRI if a MRI scan is not available or contraindicated. However, MRI is generally preferred for assessing disc bulges.
Treatment Options for a Posterior Annular Bulge
The treatment for a posterior annular bulge depends on the severity of the symptoms and the individual’s overall health. Treatment options range from conservative therapies to surgical interventions.
Conservative Treatment
For most individuals with mild to moderate symptoms, conservative treatment strategies are the first line of approach. These therapies focus on alleviating pain, reducing inflammation, and restoring mobility. Common conservative treatment options include:
- Rest: Avoiding activities that worsen the pain. It’s important to listen to your body and rest when you’re experiencing discomfort.
- Ice and heat therapy: Using an ice pack to reduce inflammation and pain, followed by applying heat to relax muscles and increase blood flow.
- Over-the-counter pain relievers: Acetaminophen or ibuprofen can help manage pain and inflammation.
- Physical Therapy: A physical therapist can guide you through specific exercises to strengthen back muscles, improve flexibility, and restore normal movement patterns.
- Chiropractic care: Chiropractic adjustments can help align the spine and reduce pressure on the nerves.
- Massage therapy: Relaxing muscles and improving blood flow.
- Corticosteroid injections: Injections of corticosteroids can be used to reduce inflammation around the affected nerve. They can provide temporary pain relief but are not a long-term solution.
- Epidural injections: These injections deliver pain medication directly into the epidural space, often providing longer-lasting pain relief compared to corticosteroid injections.
- Bracing: A lumbar support brace might be prescribed to provide support for the spine and reduce pain.
Surgical Treatment
Surgical treatment for a posterior annular bulge is usually considered a last resort option. Surgery is typically recommended if:
- Conservative treatment fails to provide relief: If pain and neurological symptoms persist despite conservative therapies, surgery may be necessary to address the underlying cause.
- Severe nerve compression: If the bulge is putting significant pressure on a spinal nerve and causing severe neurological deficits, surgery might be required to decompress the nerve root.
- Cauda equina syndrome: This is a rare but serious condition that occurs when the nerve roots at the bottom of the spinal cord are compressed. It can cause severe pain, numbness, and weakness in the legs and bowel and bladder dysfunction. Surgery is often required to relieve the pressure on these nerves.
Surgical procedures for a posterior annular bulge generally involve removing the bulging portion of the disc, which can be accomplished through a minimally invasive technique or traditional open surgery. The type of procedure will depend on the specific circumstances of the patient.
Posterior Annular Bulge: Latest Trends and Developments
Research and technological advancements are constantly evolving in the field of spinal care. New approaches and treatments are being explored to address conditions like posterior annular bulge.
Stem Cell Therapy and Regenerative Medicine
Emerging research is investigating the use of stem cell therapy to repair damaged intervertebral discs. Stem cells have the potential to differentiate into disc cells, promoting tissue regeneration and improving disc function. The use of stem cells to treat disc bulges is still in its early stage, but it holds promise as a minimally invasive and regenerative approach.
Minimally Invasive Procedures
Advances in minimally invasive techniques are enabling more precise and less invasive surgical options for treating posterior annular bulges. These minimally invasive procedures involve smaller incisions, potentially leading to faster recovery times and reduced risk of complications compared to traditional open surgeries. Laser disc decompression is an example of a minimally invasive procedure that utilizes lasers to remove bulging disc material and create space for the nerve roots.
The future of treating posterior annular bulges holds more promise for less invasive treatments and personalized care. Staying informed about these developments is important for making well-informed decisions about your health.
Tips and Expert Advice
As a blogger covering health-related topics, I understand the importance of taking a proactive approach to your well-being. Here are some tips and expert advice for managing a posterior annular bulge and maintaining a healthy spine:
- Maintain a Healthy Weight: Excess weight puts additional strain on the spine. Losing even a small amount of weight can significantly improve back health.
- Practice Good Posture: Be mindful of your posture while sitting, standing, and sleeping. Proper posture helps distribute weight evenly across the spine and reduce stress on the discs.
- Regular Exercise: Engage in regular exercise but avoid activities that worsen your symptoms. Strong core muscles can provide support for the spine and reduce pressure on the discs.
- Stretch Regularly: Stretching can help improve flexibility and reduce muscle tightness, which can contribute to back pain.
- Ergonomics: If your job requires sitting for extended periods, make sure your workstation is ergonomically designed to minimize strain on your spine. Use proper chairs, adjust desk height, and take frequent breaks to move around.
- Sleep on a Supportive Mattress: A supportive mattress can help maintain proper spinal alignment while sleeping and reduce pressure on the discs.
- Consult with a Healthcare Professional: If you are experiencing persistent back pain, numbness, or tingling, it is essential to consult a doctor or physical therapist. They can provide an accurate diagnosis, recommend appropriate treatment options, and guide you on a personalized recovery plan.
It’s important to remember that everyone’s experience with a posterior annular bulge can be different. What works for one person might not be suitable for another. It’s crucial to work closely with your healthcare provider to develop a personalized treatment plan that addresses your specific symptoms and health goals.
Frequently Asked Questions (FAQs)
Q: How long does a posterior annular bulge take to heal?
A: There’s no one-size-fits-all answer to this question. The healing time for a posterior annular bulge can vary depending on the severity of the bulge, the individual’s age, overall health, and adherence to treatment recommendations. For some people, conservative treatments might provide pain relief in a few weeks. Others might experience a longer recovery period. In some cases, the bulge might never fully heal, but the symptoms can be effectively managed.
Q: Can a posterior annular bulge go away on its own?
A: It’s possible for a posterior annular bulge to resolve on its own, especially if it’s mild and not causing significant nerve compression. However, this is not always the case. If the bulge is causing pain or neurological symptoms, it’s important to seek medical attention to prevent it from worsening.
Q: Is a posterior annular bulge serious?
A: While a posterior annular bulge might not be a life-threatening condition, it can cause significant pain and discomfort, limiting your activities and quality of life. It’s important to address the condition early on to prevent further complications.
Q: Can a posterior annular bulge lead to a herniated disc?
A: A posterior annular bulge can, in some cases, progress to a herniated disc. If the annulus fibrosus continues to weaken, the nucleus pulposus could eventually break through the annulus and herniate. Early diagnosis and treatment are vital to prevent this progression.
Q: What are the long-term implications of a posterior annular bulge?
A: If left untreated, a posterior annular bulge can lead to chronic pain and disability. It may also increase the risk of further disc degeneration and other spinal problems. Early diagnosis, appropriate treatment, and lifestyle modifications can help prevent these long-term implications.
Posterior Annular Bulge
Conclusion
Understanding the causes, symptoms, and treatment options for a posterior annular bulge is crucial for managing this common back issue. By adopting proactive measures, such as maintaining a healthy weight, practicing good posture, engaging in regular exercise, and seeking prompt medical attention, you can promote spine health and prevent complications.
If you are experiencing back pain or other symptoms that might suggest a posterior annular bulge, it’s essential to consult with a healthcare professional for a proper diagnosis and personalized treatment recommendations. Remember, early detection and intervention are key to effectively managing this condition and preventing further complications. Are you concerned about back pain or any potential spinal issues? If so, you might find this article informative.

:max_bytes(150000):strip_icc()/OrangeGloEverydayHardwoodFloorCleaner22oz-5a95a4dd04d1cf0037cbd59c.jpeg?w=740&resize=740,414&ssl=1)




