Have you ever wondered what your pelvic floor muscles do, and whether they are up to the task of keeping everything in place? The truth is, many people are unaware of the vital role these muscles play in our overall health and well-being. This article will delve into the fascinating world of the pelvic floor, exploring how professionals assess its strength and function, and why this knowledge is crucial for a range of conditions.
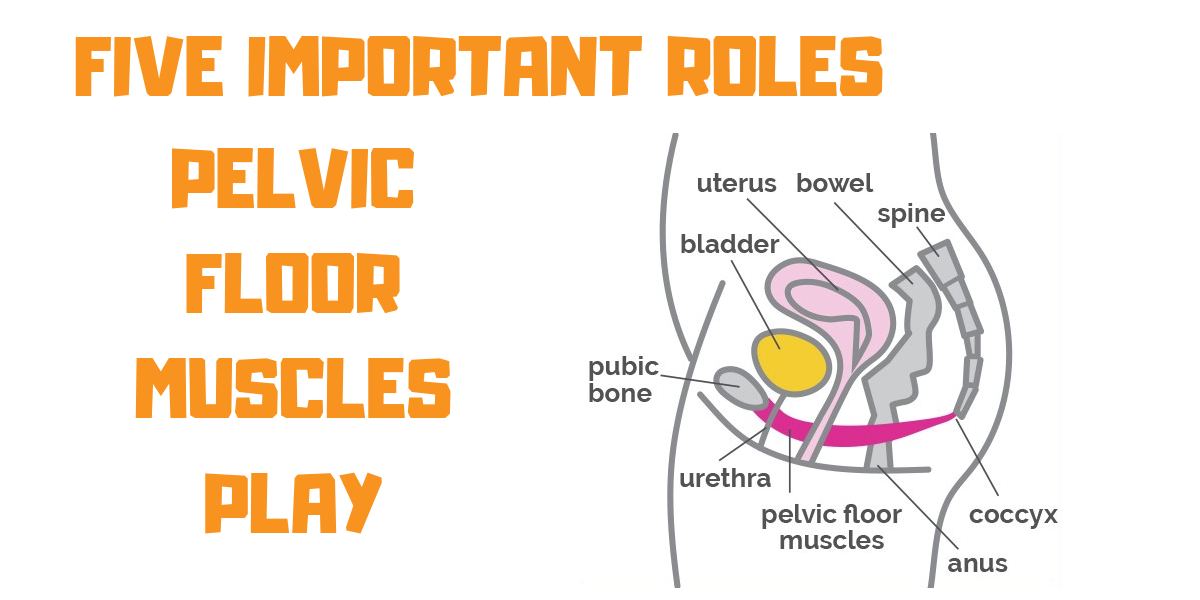
Image: infoupdate.org
The pelvic floor muscles form a sling-like structure that supports the organs in your lower abdomen, including the bladder, uterus (in women), and rectum. They are responsible for a range of essential functions, from controlling urination and defecation to supporting sexual function and even contributing to core stability. Understanding the health and strength of your pelvic floor is paramount for addressing issues like incontinence, pelvic organ prolapse, and even pain. It’s time to empower yourself with knowledge about these crucial muscles, and learn how to ensure they are working optimally for a healthier and more fulfilling life.
Unveiling the Hidden Muscles: Exploring the Pelvic Floor’s Anatomy and Physiology
To fully understand the assessment process, let’s first take a closer look at the intricate anatomy and physiology of the pelvic floor:
A Web of Muscle: The Structure of the Pelvic Floor
Think of the pelvic floor as a hammock, positioned like a sling between the tailbone (coccyx) and the pubic bone, forming the floor of the pelvis. These muscles are arranged in multiple layers, contributing to their complex and multifaceted roles. The key muscle groups include:
- The levator ani: This is the primary muscle group, responsible for supporting the pelvic organs and controlling the openings of the bladder, urethra, and rectum.
- The external anal sphincter: This muscle encircles the anus and helps regulate bowel movements.
- The external urethral sphincter: This muscle controls the flow of urine from the bladder.
The Power of Support and Control: Functions of the Pelvic Floor
The roles of these muscles extend far beyond simply holding things in place:
- Urinary and Bowel Control: The pelvic floor muscles are essential for controlling urination and defecation. They act like a valve, working to open and close the urethra and anal sphincter.
- Sexual Function: The pelvic floor muscles play a crucial role in sexual pleasure, both for men and women. They contract during orgasm and contribute to overall sexual sensation.
- Core Stability and Posture: The pelvic floor acts as a key part of the body’s core, working in conjunction with abdominal and back muscles to provide essential support and stabilization. This contributes to good posture and overall body alignment.
- Pregnancy and Childbirth: During pregnancy, the pelvic floor muscles adapt and stretch to support the growing uterus. After childbirth, they need time and effort to regain their strength and function.

Image: www.myxxgirl.com
Delving Deeper: Types of Pelvic Floor Assessments
Now that we understand the foundations of pelvic floor health, let’s examine the different ways professionals assess its strength and function.
Asking the Right Questions: The Importance of Subjective Assessment
The initial assessment often involves a thorough conversation with the patient about their concerns, medical history, and potentially relevant lifestyle factors. This is crucial for gathering information about:
- Symptoms: Understanding the specific symptoms, such as urinary incontinence, difficulty emptying the bladder, pelvic pain, or fecal incontinence, helps guide the assessment process.
- Lifestyle Factors: Factors like pregnancy, childbirth, weight changes, and chronic cough can impact pelvic floor function and need to be considered.
- Medical History: Past surgeries, pelvic floor muscle dysfunction, and other medical conditions can all influence the assessment strategy.
Hands-On Evaluation: The Physical Examination
The physical examination typically involves an internal assessment, allowing the healthcare professional to directly assess the pelvic floor muscles. While this might feel intimidating for some, it is a valuable tool for identifying both weakness and tightness in the pelvic floor muscles.
- Palpation: This involves the examiner gently pressing on the pelvic floor muscles to assess their tone, coordination, and strength.
- Visual Examination: In some cases, the examiner might use a speculum to visualize the pelvic floor muscles and assess their position and appearance.
Beyond Feeling and Seeing: Objective Assessment Tools
While subjective and physical assessments offer valuable insights, objective measurements provide additional information about pelvic floor function. Here are some commonly used tools:
- Electromyography (EMG): This test measures the electrical activity of the pelvic floor muscles. A small probe is inserted into the vagina or rectum to detect muscle activity during contraction and relaxation.
- Biofeedback: This technology provides real-time feedback on muscle activity. Patients can use biofeedback devices to learn how to contract and relax their pelvic floor muscles effectively.
- Pressure Biofeedback: This method involves inserting a small sensor into the vagina or rectum to measure pressure during pelvic floor muscle contractions.
- Ultrasound: An ultrasound scan can be used to visualize the muscles and assess their thickness, position, and movement during contraction.
Understanding the Results: What Do the Assessments Tell Us?
Once the assessment is complete, it’s time to interpret the findings and develop a tailored action plan:
Interpreting the Data: Identifying Strengths and Weaknesses
The assessment results provide valuable information about the overall health and function of the pelvic floor muscles. This includes:
- Muscle Strength: Are the muscles strong enough to support the pelvic organs and control sphincter function?
- Muscle Control: Can the muscles be consistently and effectively contracted and relaxed?
- Muscle Coordination: Are the different muscle groups working together efficiently?
- Trigger Points: Are there any areas of muscle tension or tightness that could be contributing to pain or dysfunction?
Tailoring Treatment: Addressing Specific Issues
Based on the assessment results, a healthcare professional can tailor a specific treatment plan to address:
- Pelvic Floor Muscle Weakness: This can be addressed with targeted exercises, known as pelvic floor muscle training, to strengthen and improve control.
- Pelvic Floor Muscle Tightness: This can involve relaxation techniques, stretching exercises, and manual therapy to relieve muscle tension and improve flexibility.
- Coordination Issues: This can be addressed with biofeedback therapy to help individuals learn proper muscle engagement and coordination.
- Pelvic Organ Prolapse: Treatment might involve pelvic floor muscle training, pessary devices (to support the pelvic organs), or surgical interventions depending on the severity of the prolapse.
- Urinary Incontinence: Treatment might include pelvic floor muscle training, bladder training, medications, or surgery depending on the cause and severity of incontinence.
Empowering Yourself: Taking Control of Your Pelvic Floor
Regardless of your age or gender, understanding your pelvic floor health is empowering. Here are some practical tips for maintaining optimal pelvic floor function:
- Engage in Regular Pelvic Floor Muscle Training: This involves consciously contracting and relaxing the pelvic floor muscles, similar to the way you might squeeze and release a muscle in your arm.
- Practice Proper Lifting Technique: Avoid straining your pelvic floor when lifting heavy objects. Proper form and a strong core are crucial for minimizing strain.
- Maintain a Healthy Weight: Excess weight puts additional strain on your pelvic floor muscles. Losing weight can significantly reduce the risk of dysfunction.
- Avoid Smoking: Smoking can weaken your pelvic floor muscles and increase the risk of incontinence.
- Stay Hydrated: Adequate fluid intake is crucial for bladder health and the overall function of your pelvic floor.
Assessment Of Pelvic Floor Muscle Strength And Function
https://youtube.com/watch?v=JoypO7Tm_Js
Conclusion: A Journey of Understanding and Empowerment
By understanding the importance of pelvic floor function and exploring various assessment techniques, we can gain invaluable insights into the health of these often-overlooked muscles. Whether you are experiencing symptoms or simply hoping to maintain optimal function, seeking professional guidance is essential. The journey towards a healthier and more empowered life begins with understanding and addressing your pelvic floor needs. This journey starts with you, and with the right knowledge and support, it can lead to a more fulfilling and comfortable life.

:max_bytes(150000):strip_icc()/OrangeGloEverydayHardwoodFloorCleaner22oz-5a95a4dd04d1cf0037cbd59c.jpeg?w=740&resize=740,414&ssl=1)




