Imagine this: you’re bending over to pick up a dropped item and a sharp pain shoots through your lower back. You instinctively grab your back, wincing at the sudden discomfort. This familiar scenario, while seemingly simple, could be a sign of a deeper issue – SI joint dysfunction. And while this pain might be localized to your lower back, it can have unexpected consequences, potentially impacting the intricate network of muscles that support your pelvic floor.
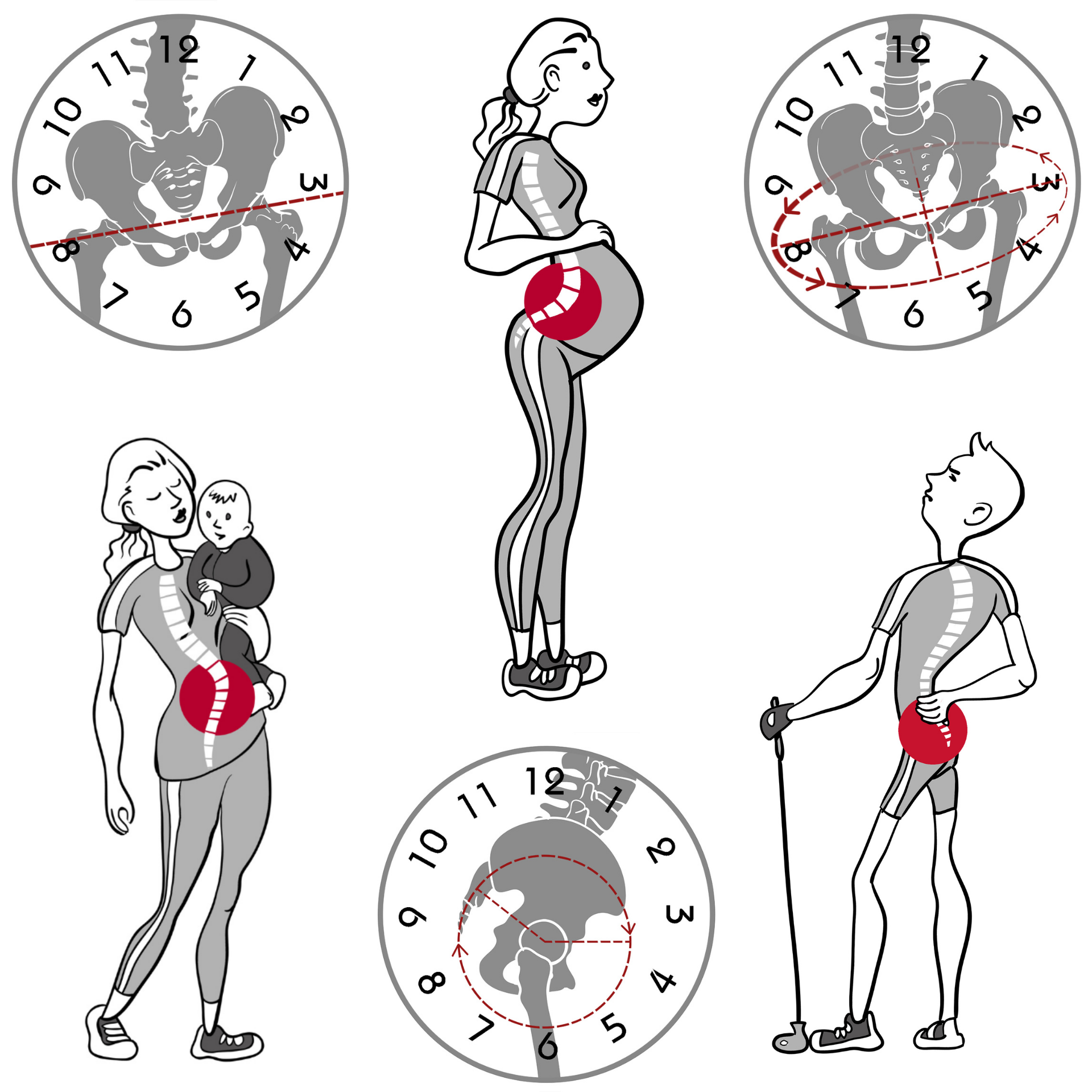
Image: deborahsilvermusic.com
The sacroiliac (SI) joint, nestled between your sacrum (the triangular bone at the base of your spine) and your ilium (the largest bone in your pelvis), plays a crucial role in stabilizing your pelvis and transferring weight from your upper body to your legs. When this joint becomes irritated or inflamed, it can trigger a cascade of events affecting not only your back but also your pelvic floor muscles. Understanding this connection is critical for those experiencing pelvic floor dysfunction, as often, the root cause can be surprisingly found outside the pelvis itself.
Understanding the SI Joint and Its Connection to Pelvic Floor Dysfunction
The SI joint, although small in size, is a highly complex structure. It’s designed to accommodate a wide range of movement while maintaining stability. This delicate balance can be disrupted by various factors, including injury, pregnancy, repetitive strain, and postural imbalances. When the SI joint becomes misaligned or inflamed, it can trigger a chain reaction, leading to pelvic floor dysfunction.
1. Pain Referral: A Backache with Pelvic Consequences
A common phenomenon associated with SI joint dysfunction is *pain referral*. This means that the pain originating from the SI joint can be perceived in other areas of the body, including the pelvic floor. The pain signals are relayed through the nervous system, causing a sensation of discomfort and tightness in the pelvic region, mimicking the symptoms of pelvic floor dysfunction.
2. Muscle Imbalances: A domino effect on the pelvic floor
SI joint dysfunction can throw off the delicate balance of muscles in the lower back, pelvis, and hips. This disruption can affect the way you move and stand, leading to a cascade of muscle imbalances. The pelvic floor muscles, intricately connected to the muscles around the hips and lower back, are particularly susceptible to these imbalances. When the SI joint is not functioning optimally, the surrounding muscles might overcompensate, leading to tightness, tension, and ultimately, pelvic floor dysfunction.

Image: www.physiomed.ca
3. Altered Mechanics: A Ripple Effect on Pelvic Floor Function
The SI joint plays a pivotal role in stabilizing your pelvis and transferring weight effectively. When the joint is compromised, these mechanics are disrupted, affecting the way your entire body moves and supports itself. This alteration in biomechanics can impact the ability of the pelvic floor muscles to function correctly. For example, a misaligned SI joint might lead to an uneven distribution of weight, placing undue stress on the pelvic floor muscles, contributing to dysfunction.
Pelvic Floor Dysfunction: A Multifaceted Problem
Pelvic floor dysfunction is not a singular condition but rather a broad umbrella encompassing various issues related to the muscles, nerves, and tissues of the pelvic floor. These issues can manifest in a multitude of ways:
- Urinary incontinence: Involuntary leakage of urine.
- Fecal incontinence: Difficulty controlling bowel movements.
- Pain during intercourse: Dyspareunia, a common symptom experienced by both men and women.
- Pelvic pain: Chronic pain in the pelvic region, often associated with tension and tightness in the pelvic floor muscles.
- Difficulty emptying the bladder: Feeling like you can’t fully empty your bladder, a condition known as urinary retention.
- Prolapse: A condition where organs in the pelvic region, such as the bladder or rectum, descend into the vagina.
How to Identify a Potential SI Joint Connection
While there is a potential link between SI joint dysfunction and pelvic floor dysfunction, it’s crucial to identify the root cause. It’s best to consult a healthcare professional, such as a physical therapist or pelvic floor specialist. There are various tests and assessments to help identify if your SI joint is contributing to your pelvic floor issues. Some of these include:
- Physical examination: A thorough examination by a healthcare professional can reveal any tenderness, pain, or movement limitations in your SI joint.
- Palpation: Gently pressing on the SI joint to assess for tenderness and pain.
- Range of motion tests: Evaluating the range of motion in your hips, pelvis, and lower back to identify any restrictions that might indicate SI joint dysfunction.
- Special tests: There are specific tests, such as the Gaenslen test or the SI joint compression test, that are designed to assess and diagnose SI joint dysfunction.
- Imaging studies: In some cases, imaging studies like X-rays or MRIs might be used to rule out other conditions or provide further confirmation of SI joint dysfunction.
Addressing the Issue: A Multi-pronged Approach
Once a diagnosis is established, a tailored treatment plan will be developed to address the underlying cause and its impact on your pelvic floor. This may involve:
- Manual therapy: Physical therapists employ techniques like massage, stretching, and mobilization to restore proper function to the SI joint, improve mobility, and reduce pain.
- Exercise: Specific exercises help strengthen the muscles around the SI joint, improve stability, and enhance pelvic floor function. This might include core strengthening exercises, hip mobility exercises, and gentle stretches targeting the lower back.
- Postural correction: Training your body to maintain proper posture is instrumental in relieving strain on the SI joint and reducing the risk of further dysfunction.
- Pelvic floor therapy: Working with a pelvic floor specialist can address specific abnormalities in your pelvic floor muscles, teaching you exercises to improve strength and control.
- Lifestyle modifications: Adjusting activities like lifting, sitting, and walking can reduce stress on the SI joint and prevent further strain.
- Pain management: Medications, heat therapy, and other pain-relief strategies may be recommended to manage pain and discomfort arising from SI joint dysfunction.
Preventing Future Issues: A Holistic Approach
Proactively addressing factors that contribute to SI joint dysfunction, such as poor posture, repetitive strain, and inadequate muscle support, can significantly reduce the risk of future issues. Here are some preventive measures to consider:
- Maintain good posture: Focus on maintaining an upright, balanced posture, especially when sitting or standing for prolonged periods. Correcting slouching and ensuring your back is supported can alleviate stress on the SI joint.
- Strengthen core muscles: A strong core provides crucial support to your spine and pelvis. Engage in regular exercises to strengthen your abdominal muscles, lower back muscles, and pelvic floor muscles.
- Improve flexibility: Regularly stretching your hips, lower back, and pelvic floor muscles can improve mobility, create balance, and reduce stiffness. This can be beneficial in preventing future SI joint dysfunction.
- Practice safe lifting techniques: Using proper techniques when lifting heavy objects helps to reduce strain on your back and prevent injuries. Always bend your knees, keep your core engaged, and avoid twisting your body while lifting.
- Avoid repetitive strain: If your job or hobbies involve frequent repetitive movements, consider taking regular breaks to stretch and move around to reduce strain on your SI joint.
Can Si Joint Cause Pelvic Floor Dysfunction
Conclusion
While the link between SI joint dysfunction and pelvic floor dysfunction is not always straightforward, it’s a connection worth exploring. Recognizing the potential influence of the SI joint on your pelvic floor health can lead to a more comprehensive approach to treating pelvic floor dysfunction. By seeking professional guidance, understanding the intricate connections, and implementing appropriate strategies, you can address the root cause of your pelvic floor issues and regain control over your body’s overall well-being.

:max_bytes(150000):strip_icc()/OrangeGloEverydayHardwoodFloorCleaner22oz-5a95a4dd04d1cf0037cbd59c.jpeg?w=740&resize=740,414&ssl=1)




